A Pox on Our Nation
It’s been more than nine decades since Canada had its last brush with a deadly smallpox epidemic. When the dreaded disease broke out in southwestern Ontario’s Windsor region in early 1924, almost half of the sixty-seven people who contracted the illness died. Doctors were taken by surprise and at first failed to identify it. Canada had not seen such a serious smallpox epidemic since 1885, when the illness swept Montreal, killing 3,154 people.
“Today we have no conception of the meaning of the word ‘smallpox,’” wrote Dr. John Heagerty of Canada’s Federal Public Health Service in a booklet published shortly after the Windsor outbreak. “For us the word has been robbed of its terrors, and we discuss the problem of smallpox in the community in a general and academic way.”
But the illness was hardly academic to those who were stricken. The Windsor outbreak in January was traced to the home of furniture mover Gordon Deneau. None of the four doctors who saw Deneau initially recognized his ailment as a particularly virulent form of hemorrhagic (bloody) smallpox. After Deneau’s death, more people became sick. Five members of his immediate family died. Once doctors knew what they were dealing with, measures were quickly put in place.
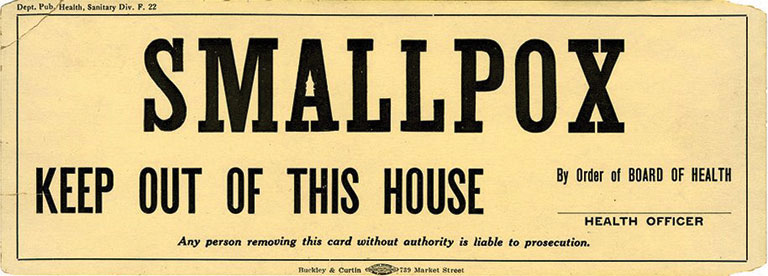
Patients were quarantined, and within a week most of the seventy thousand people in the Windsor area were vaccinated, effectively stopping the epidemic in its tracks. “All deaths which occurred were of unvaccinated persons,” reported Toronto’s Globe in March 1924. “The only persons who attended the funeral of Deneau and escaped infection were those vaccinated.”
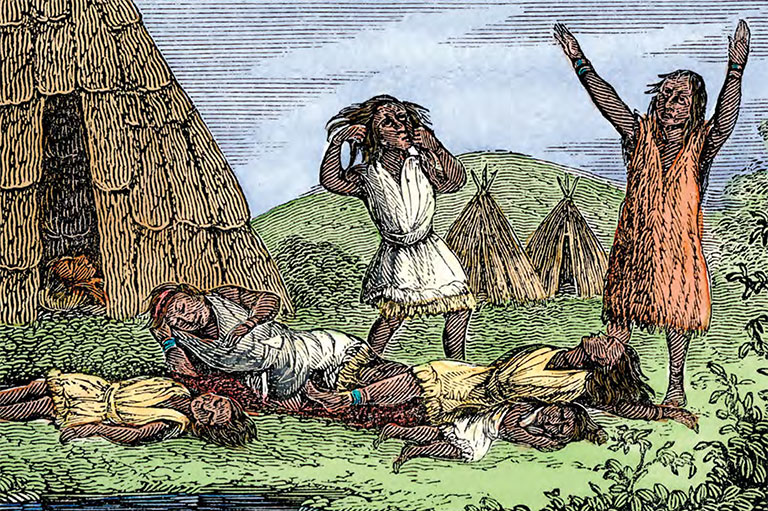
In pre-vaccine days, noted Heagerty, “the word ‘smallpox’ blanched the cheek and brought a look of terror to the eyes. Smallpox in those days meant death. Relentless and insatiate, the disease would sweep through a community mowing down all those who had not already suffered from it; killing, maiming, and leaving its victims blinded or disfigured for life.” Moreover, “it played a part of no little importance in the political history of Canada in the early days.”
Although officially eradicated in 1979, smallpox remains a threat today, either as a potential bioterrorist weapon or as a virus inadvertently resurrected. In recent years scientists have speculated that the virus could spread from the frozen bodies of eighteenth-century victims of the disease that thaw as global warming melts the Siberian permafrost. Thus it’s worth giving the subject of smallpox some thought today.
Smallpox began to shape Canada’s political history in 1616 when the disease struck the Indigenous population living near Tadoussac, France’s first North American fur-trading post. The disease had been unknown to the First Nations, who had no natural immunity, and this population would become highly vulnerable to its deadly power.
However, there is more to the first chapters of the Canadian smallpox story than its devastating impact on the indigenous population. During the pre-Confederation era the effects of smallpox varied over time and geography. Its severity, spread, control, and ultimate prevention through quarantine and immunization were shaped by many factors. French and British settlers, and the traders of the Hudson’s Bay Company in North America, all had different political and economic goals and cultural perspectives that affected how they responded to smallpox.
Characterized as the “speckled monster,” smallpox first emerged as a pandemic disease threat in ancient East Asia and then spread through the Middle East, India, Africa, and Europe. It is an acute, contagious, self-limiting, and naturally immunizing infectious disease caused by two virus types — Variola major and the less severe Variola minor.
The virus spreads through infected droplets and contact with infectious rashes and blisters. It starts with flu-like symptoms — such as fever, cough, aching joints — then proceeds to rashes and blisters that appear first inside the mouth and then on the skin, starting on the face and spreading down the body. The blisters rupture, spew pus, and eventually crust over, leaving permanent scarring.
In severe Variola major cases the virus attacks the vital systems of the body, including the eyes, leading to serious complications, such as blindness, and often death. The mortality rate generally ranges between thirty and thirty-five per cent but can be much higher, as it was in Windsor in 1924. Those who survive receive lifelong immunity.
The earliest reported smallpox epidemic in the western hemisphere struck in the West Indies in 1507, likely introduced by Spanish sailors. The Spanish importation of African slaves who were infected with smallpox intensified the impact of the disease, as did the fact that the indigenous people of what today is known as Latin America tended to be concentrated in cities. Thus, smallpox spread rapidly, with devastating results.
With 7 uniquely curated newsletters to choose from, we have something for everyone.
Remarkably, smallpox would not be introduced north of what is today Mexico for another century. French and British settlers brought the disease to the fledgling New France and New England colonies, followed by Dutch traders who would inadvertently spread it north and west. At the time about three million Indigenous people lived north of Mexico in populations that, unlike their counterparts further south,were mostly nomadic and thinly spread.
From the St. Lawrence River trading post of Tadoussac in 1616, the disease soon spread to other tribes in the Maritimes, James Bay, and Great Lakes regions. At about the same time, smallpox arrived with British settlers in the Boston Bay area, soon eliminating almost ninety per cent of the local Massachusetts tribes of the Algonquin nation. From the Puritans’ perspective, this was divine providence, since it cleared the way for settlement. “For the natives, they are all near dead of the smallpox, so the Lord hath cleared our title to what we possess,” declared local Governor John Winthrop in a 1634 letter.
While British settlers would establish an antagonistic relationship with Indigenous people through an increasingly violent clash over land, Dutch traders were drawn into a close economic relationship with Indigenous tribes that attracted traders north and west towards the St. Lawrence and Great Lakes, unknowingly bringing smallpox with them. During the 1630s nearly every tribe in the Great Lakes region was affected by smallpox, and by 1636 the population of the Huron north of Lake Ontario had been reduced by half after a four-year epidemic.
The Huron blamed French Jesuit missionaries for the plague. The Jesuits may have been responsible for some spread of the disease, but most of them would have been immune from previous exposure in France.
A Jesuit Relations entry from 1637 explains how one outbreak got started: “It was upon the return from the journey which the Hurons made to ‘Kebec’ that it started in the country — our Hurons, while again on their way up here, having thoughtlessly mixed with the Algonquins, whom they met on the route, most of whom were infected with smallpox. The first Huron who introduced it came ashore at the foot of our house, newly built on the bank of a lake — being carried thence to his own village, but a league distant from us, he straightaway died.”
Unlike the English and Dutch settlers and traders, the French missionaries did their best to care for the stricken Hurons. But they could do little as the Huron, weakened by disease, became more vulnerable to attack by their Iroquois rivals. By 1650 the Huron had ceased to exist as a nation in their territory. Survivors either joined the Iroquois or took refuge in Quebec.
During the balance of the seventeenth century, smallpox was present among the Indigenous population as it spread over half of North America, taken in all directions as whole tribes fled in terror during epidemics. The speckled monster would also play a major role in shaping the course and outcome of wars between the English and French for control of North America.
In 1690, for example, an invading army of New England troops and their First Nations allies were planning a siege of Montreal and Quebec via Lake Champlain when smallpox outbreaks struck as the sailing forces landed near Quebec. Smallpox also spread among a marching land force while it approached Montreal, leaving hundreds of soldiers dead from the disease.
Yet smallpox did not play favourites; it similarly sabotaged an ambitious French plan in 1746 to recapture Louisbourg and Annapolis and also attack the English settlements along the east coast. The plan involved troops from New France and a large force sailing from France to join up at Chebucto in present-day Nova Scotia. During the ninety-day voyage the French fleet lost 1,270 men to disease and shipwreck, and then it lost another 1,130 after landing at Chebucto. Local Mi’kmaq who were drawn to Chebucto for supplies quickly became infected, resulting in an epidemic that left more than a third of the tribe dead.
It has been suggested that smallpox was used as a biological weapon against First Nations, especially during the 1750s and 1760s in the midst of the wars between the English and the French. There certainly was some thought of doing so.
It started in 1757, when a French force led by Louis-Joseph de Montcalm attacked Fort William Henry in what is now New York State. After taking the fort, Montcalm’s First Nations allies attacked the English soldiers who had given up and were leaving the fort. And, despite Montcalm’s efforts to stop them, the warriors also plundered the fort, which was unsanitary and rife with smallpox. When the illness later broke out among the First Nations, it appeared to them to be an act of retribution by the English.
According to Montcalm, “fortunately they [the Indians] had frequently declared in the different councils held at Michilimackinac and Detroit that the English had thrown that medicine [smallpox] on the Indians which they might have turned aside if they had been willing to believe the French General and not plunder the baggage of the English.”
There was definitely contempt for the First Nations among the English after what happened at Fort William Henry. Not long after, the idea of using smallpox as a weapon came up as a postscript in correspondence between British military leader Jeffrey Amherst and one of his colonels, “Could it not be contrived to send the smallpox among those disaffected Indians?” wrote Amherst.
In a reply to Amherst dated in July 1763, Colonel Henry Bouquet wrote, “I will try to inoculate them with some blankets that may fall in their hands and take care not to get the disease myself.” While it is possible to spread the disease through blankets or other articles contaminated with fresh scabs from smallpox victims, there is no evidence that such plans were ever deliberately carried out.
Smallpox among First Nations was of considerable concern to the traders of the Hudson’s Bay Company as they expanded westward.
Meanwhile, the English also accused Montcalm of using smallpox as a weapon. They claimed that Montcalm tried to spread the disease among the British by sending the prisoners of Fort William Henry to Halifax on a ship on which smallpox had broken out.
Soon after the British conquest of New France in 1763, a new biological weapon emerged in the smallpox war. This weapon was known as smallpox variolation — a method of preventing the disease by exposing people to it in a controlled manner. Variolation originated in eleventh-century China and India and was based on the observation that most people who contracted smallpox never caught it again.
It appeared that if a person became infected through a scratch they developed a much less severe form of the disease than those who were infected by the more usual oral route of the virus. By the mid-eighteenth century, variolation was widely used in Europe, although there was significant resistance to it, as it often failed to work.
Variolation was first used in British-held Quebec in 1765, and by 1769 a concerted immunization effort had been launched among the prominent English and French families in Montreal and Quebec and also most of the British troops stationed in the colony.

The Thirteen Colonies were much slower to take up variolation, however. There were religious concerns about the practice interfering with God’s providence — the same providence that had cleared the land for the English settlers by killing off the indigenous people. There was also medical and scientific mistrust about the method’s safety and effectiveness. Thus, variolation was severely restricted or banned in most of the Thirteen Colonies. This proved to be a disadvantage when the American Revolution broke out in 1775.
British troops and Canadians north of the St. Lawrence River were significantly more immune to smallpox than the revolutionaries to the south. And, while General George Washington attempted to variolate his troops in the Boston area in 1775, the effort proved to be too little, too late. When he launched his attack on Quebec in July 1775, smallpox broke out among Washington’s troops; yet the disease did not affect the immunized British forces, forcing Washington’s men to retreat hastily. It was clear that smallpox played a major role in saving Canada for the British Empire.
Variolation also benefited the Indigenous population of British North America. British colonial authorities allowed the Mohawk living near the Kingston area of Upper Canada to be variolated starting in 1796. Smallpox immunization through variolation would continue in British North America until the 1850s, although this method would be supplanted by smallpox immunization through vaccination, a more effective approach to preventing the disease that was developed by Edward Jenner in Britain in 1796 and first used in North America shortly thereafter.
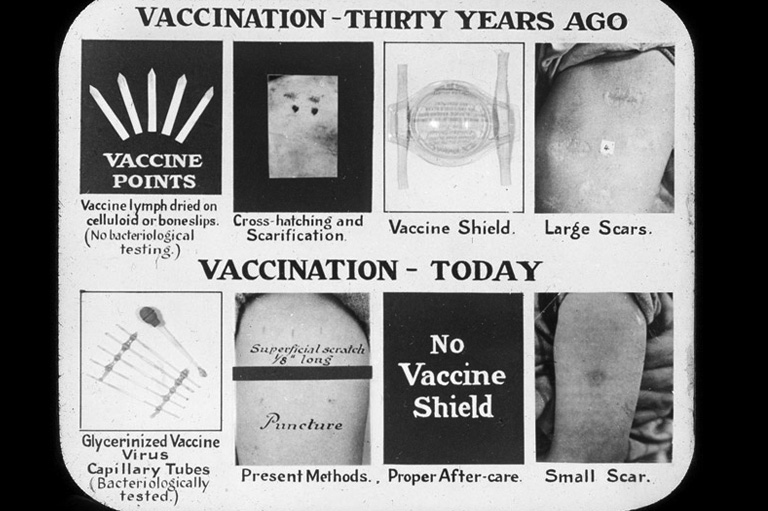
Jenner observed that milkmaids rarely had pox-marked skin and discovered that exposure to a mild cowpox infection (vacca is Latin for cow) effectively immunized people against smallpox. Although not the first to make this observation, Jenner was the first to collect the cowpox-infected material from the skin of calves to prepare a “vaccine” and then to clearly demonstrate that the inoculation of a healthy person protected them from the disease during a smallpox outbreak.
British North American Indigenous peoples quickly benefited from smallpox vaccination and were enthusiastic about its value. The first were vaccinated in 1803 after travelling hundreds of kilometres to receive it. In 1807, Jenner personally sent a supply of smallpox vaccine to the Five Nations Indians at Fort George along with the formal gift of his book about vaccination to help explain how it worked. The chief of the Five Nations Indians received the gift with great appreciation and wrote back to thank Jenner. “We send with this a belt and string of Wampum in token of our acceptance of your precious gift, and we beseech the Great Spirit to take care of you in this world and in the land of spirits.”
Smallpox vaccination saved many in the Canadian Indigenous population, but it would take time for its benefits to be applied evenly. Smallpox continued to be imported from the United States,where vaccination was adopted more slowly. And having a sufficient vaccine supply was a major challenge.
Smallpox among First Nations was of considerable concern to the traders of the Hudson’s Bay Company (HBC) as they expanded westward. A major epidemic swept across the West from 1780 to 1782, and HBC traders often witnessed its devastating impact. For instance, in the fall of 1781, Mitchell Oman, an HBC fur trader, met a group in the Eagle Hills region of present-day Saskatchewan who had barely survived an attack of smallpox. Looking into their tents, he saw that most were dead. He later reached Fort Buckingham at present-day Elk Point, Alberta, and discovered that “all was solitary silence ... there was no Indian to hunt for us ... three-fifths had died.”
When William Tomison, another HBC trader, arrived at York Factory on Hudson Bay in early July 1782, he confirmed the news of the smallpox epidemic in the interior. He was being followed to the fort by six canoes of Indigenous people carrying their season’s furs, but three were ill with smallpox and eventually died. With this news, word was immediately sent to the local First Nations living near York Factory, telling them not to visit the fort.
Shortly after, three more First Nations ill with smallpox approached from the interior, but they were met before reaching the fort by an HBC trader. They were given food and medicine and were persuaded to set up their camp six kilometres upstream. All three died, but, due to this early quarantine effort, they and the earlier three were the last Indigenous deaths from smallpox recorded in the York Factory journals, which continued until 1949.
It was a similar story during the epidemic that struck Cumberland House in 1781–82. There, Tomison and his men demonstrated their compassion for the stricken Indians. They took them into their already crowded quarters and provided them with food, shelter, and twenty-four-hour care. They also dug graves in the frozen ground for the fatal cases.
In 1837, a second great smallpox epidemic was imported into the Canadian prairies via the Missouri River. It was caused by the arrival in June of an American Fur Company steamboat in Fort Union, a major fur trade post on the present-day North Dakota-Montana border. A deckhand ill with smallpox was allowed to leave the ship, causing the disease to spread quickly to nearby indigenous people who came to trade at Fort Union.
By September, word of the spread of “some bad disease” reached Dr. William Todd, a surgeon and the HBC chief factor of the Swan River district, near the present-day border of Manitoba and Saskatchewan. Todd, who had recently received a fresh supply of vaccine from England, guessed correctly that the disease was smallpox. He immediately vaccinated sixty First Nations living in the vicinity of Fort Pelly, and he also taught them the technique of arm-to-arm vaccination, so that they could vaccinate others.
In arm-to-arm vaccination, as soon as a cowpox postule appeared on a vaccinated person’s arm, material from the lesion was removed and used to vaccinate another person. Todd also sent fresh vaccine to other HBC factors, resulting in the company being able to stem the northward spread of the illness.
Over the next two years, the company took further steps to keep the disease at bay, launching a massive vaccination program with the goal of inoculating every person within its domain. Thus the Hudson’s Bay Company ended up serving as the de facto public health agency across western Canada during the late eighteenth and early nineteenth centuries.
The effort would limit the disease to little more than a toehold for several decades. The systematic project was accomplished with relatively little difficulty due to the HBC’s efficient transportation systems and organizational structure, something the United States could not match at the time.
It was a sharply different story across the U.S. plains, where limited inoculation efforts were carried out. By the time the 1837 epidemic died out in the winter, several tribes were devastated. The situation changed after 1840, when the U.S. government began a program to vaccinate the surviving Indigenous population.
This effort soon created a situation where the Indigenous population was better protected from smallpox than other Americans. In fact, many of the latter refused the vaccine. This, plus conditions exacerbated by the slave trade and the Civil War, fuelled a long series of severe epidemics among non-Indigenous during the mid-to-late nineteenth century.
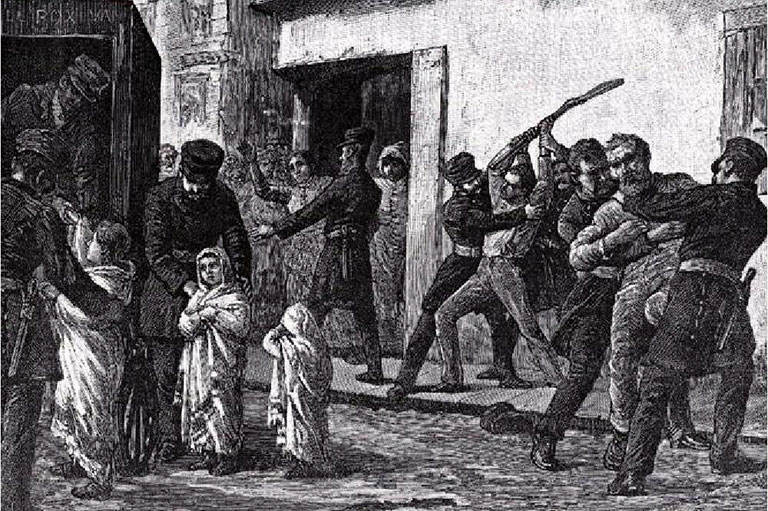
There was similar vaccine resistance in Canada during this period, but it was more limited and focused on the French-Canadian community in Quebec. Opposition was driven as much by tensions in English-French relations as by medical concerns. For instance, anglophone factory owners advocated compulsory vaccination for their French-Canadian workers, leading some francophones to view vaccination as a race weapon used by the English against the French.
One prominent doctor, Joseph Emery-Coderre, spoke out strongly against vaccination, in large part because two of his own eleven children had died shortly after being vaccinated. The fact that the city’s original vaccination program had to be suspended because of tainted vaccine did not help the cause. Thus, by the time the 1885 epidemic broke out in Montreal, vaccine resistance was at its peak — only about one sixth of the population of that city had been vaccinated.
Further west, in the colonies of British Columbia and Vancouver Island, yet another response played out when a major smallpox epidemic struck in 1862–63. The epidemic was introduced after a steamer from San Francisco arrived in Victoria bearing a passenger who had developed smallpox en route.
In the absence of clear leadership and authority to control the disease, the ill passenger was allowed to leave the ship, and the disease spread. Smallpox soon reached an area known as the northern encampment, where coastal First Nations had settled. Since they had no previous exposure to smallpox, the illness spread rapidly among them.
The colonists did little other than to express pity for the victims and to press for self-interested measures designed to insulate colonists from the infected First Nations. Indeed, not unlike when smallpox first struck in Boston Bay in 1616 and was seen by the British colonists as divine providence that cleared the land for cultivation, many of the Victoria colonists took advantage of the situation to clear the area of Indigenous people. Tsimshian, Songhee, Stikenes, and Haida people living in the northern encampments were evicted. Those who fled dispersed to their coastal homelands, spreading smallpox further across the two colonies.
Smallpox vaccination was easily available in Victoria and New Westminster, but outside these cities the vaccine was expensive and difficult to obtain. Its application among the indigenous population by missionaries and government officials was sporadic and in most cases was provided too late to do much good.
Efforts were made by Hudson’s Bay Company officials based in Fort Rupert to vaccinate more than a hundred Indigenous people around the fort. A similar initiative took place around Fort Kamloops. There were also reports of some First Nations attempting to vaccinate themselves. Nevertheless, nearly fourteen thousand people, most of them indigenous, died of smallpox on the coast alone.
Ultimately, as historian Robert Boyd has stressed, smallpox “served as a final blow to the Native peoples of British Columbia and paved the way for the colonization of their lands by peoples of European descent.”

In the twentieth century, Canadian scientists played significant roles in the World Health Organization’s campaign to eradicate the disease from the planet. It was officially declared eradicated in 1979.
With the end of smallpox came the end of mass smallpox vaccination programs. Connaught Laboratories in Toronto began the process of shutting down its smallpox vaccine production facility. The last lots of vaccine were completed in March 1980 for a proposed stockpile, but the stockpile plan was soon cancelled, and a set of fifteen vaccinia pulps, the primary ingredient for making the vaccine, were put in deep-freeze storage along with the seed virus. A final shutdown was scheduled and included plans for the incineration of the remaining pulps and materials.
In September 1980, however, Connaught’s medical director, Dr. E.W. Pearson, strongly recommended that the frozen pulps be kept. As he stressed, “It surely will not be a great problem to keep the seed virus and pulps for some time to come, and at least in this way we might have something to fall back on so as to be able to prepare our licensed product.”
The vaccinia pulps were indeed saved and kept in the deep freeze, undisturbed, for the next twenty-one years. Then came the terrorist attacks of September 11, 2001, which led to concerns about smallpox being used as a bio-terrorist weapon.
The vaccina pulps were retrieved, and Canada has since created a new smallpox vaccine stockpile. The Canadian Public Health Agency has a contingency plan in place should a new outbreak occur. This is a good thing, since much of the world’s population is now as vulnerable to smallpox as Canada’s Indigenous population was four hundred years ago.
Microscopic Killers
From earliest times it was understood that some illnesses were spread from person to person, but how this happened was a mystery. Bacteria were first observed under the microscope by Dutch scientist Anton van Leeuwenhoek in 1673. In 1762, Viennese physician M.A. Plenciz published a germ theory of disease. A century later the theory was demonstrated by French chemist Louis Pasteur and others. Yet strong opposition to the idea that micro-organisms — such as bacteria, viruses, fungi, and prions — cause disease continued and persists even today.
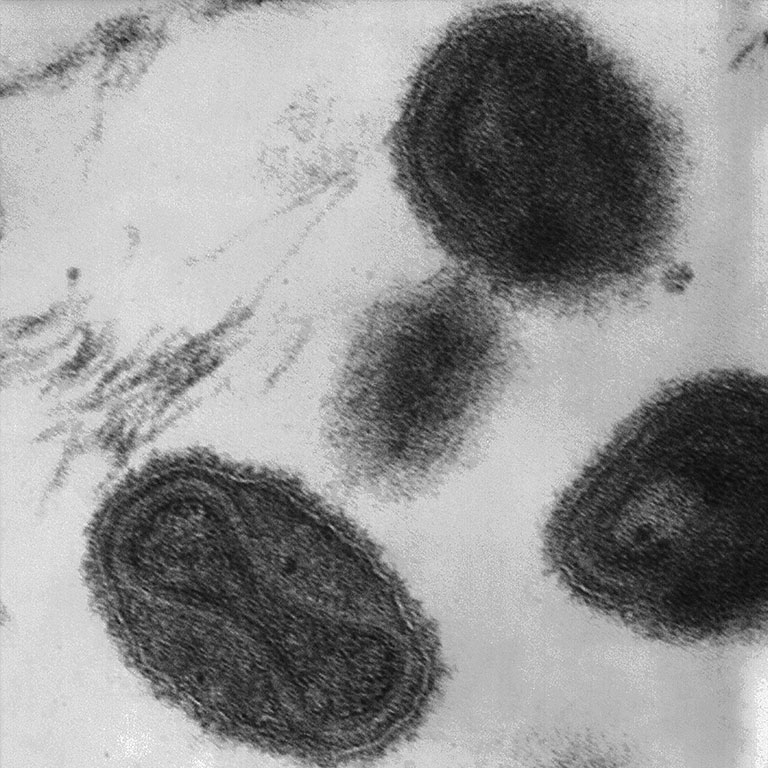
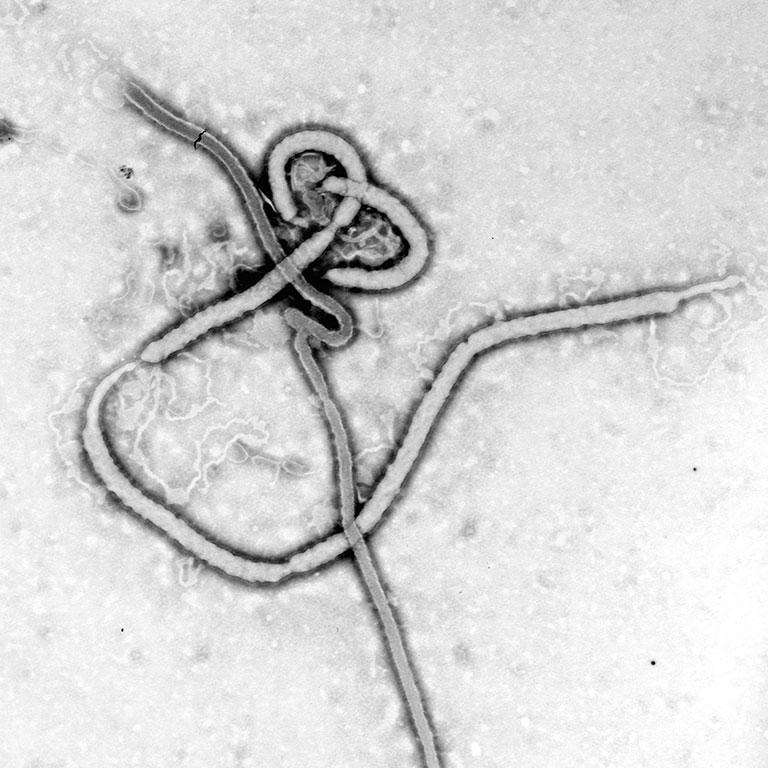
Smallpox
While smallpox was known for centuries, the Variola virus associated with it was not identified until 1906 by Italian pathologist Adelchi Negri. Like other viruses, it can only been seen under an electron microscope.
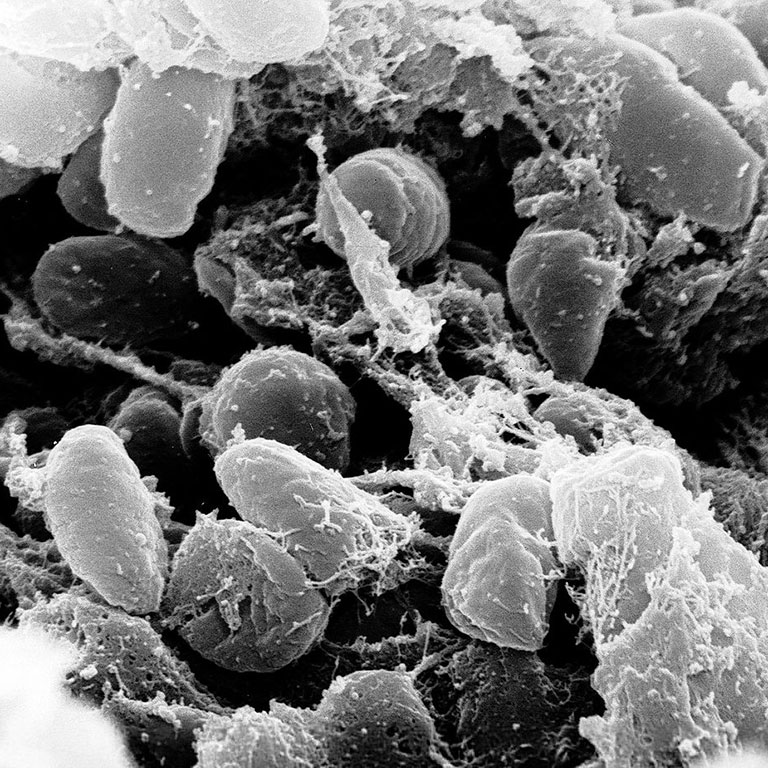
Bubonic Plague
Known as the dreaded Black Death in medieval times, bubonic plague is an infection caused by the Yersinia pestis bacterium. It is generaly spread by infected rat fleas. Plague still occurs today, but it is treatable with antibiotics.
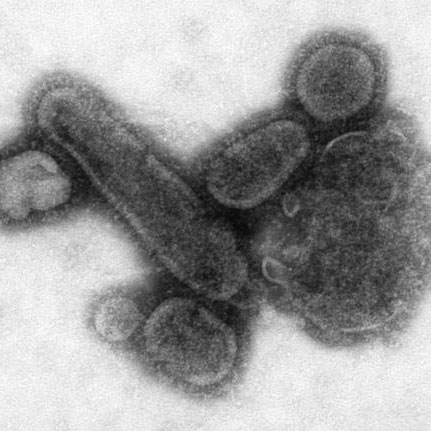
1918 Pandemic
The 1918 influenza epidemic killed about fifty million people worldwide. It involved a deadly strain of the H1N1 virus. In a controversial move, scientists recently reconstructed the viral strain for research purposes.
Ebola
The deadly hemorrhagic illness caused by the Ebola virus was first seen in remote villages in central Africa in 1976. The outbreak in 2014–2015 is the largest to date. Canada has been at the forefront of developing a vaccine.
Themes associated with this article
Advertisement
You might also like...
Canada’s History Archive, featuring The Beaver, is now available for your browsing and searching pleasure!