The Crusader

Dr. William John McKay sat back in his chair and fixed his gaze on each member of the Saskatoon Board of Health in turn. It was November 6, 1911. Before him on the table were the results of his investigations as the city’s medical health officer (MHO) into the outrageously unsanitary conditions of many local slaughter houses.
Too many butchers, he had found, chose to flout the city’s health regulations and repeatedly ignore his department’s demands for improvements. From the reports he submitted to that meeting, we might imagine the scene.
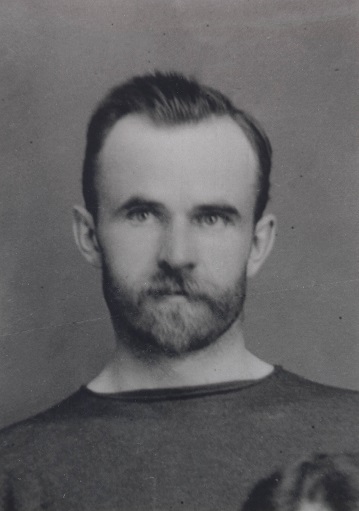
A trim, athletic man with dark hair and a neat beard, Dr. McKay holds up a sheaf of papers. “You can see for yourselves, gentlemen,” he begins, “we have made no progress with the firm of Gordon and Sparling. Hogs intended for slaughter are feeding and wallowing in dirty blood and water from the killing room. The slop from the hog trough flows toward the river, polluting the ground for hundreds of feet.”
With his index finger, the MHO thumps the tabletop for emphasis.
“The offal wagon is open, coated with dung and blood, and leaking liquid filth. Maggots and flies abound. The water supply is a shallow well less than twenty feet from the slaughterhouse which is itself a cheap shell with a defective wooden floor and poor lighting. The place is littered with hair, blood, dung, and fat. The men’s overalls, knives, and knife sheaths are greasy and caked with blood. Dogs run freely, drinking from the pails and sniffing the carcasses which, once dressed, are exposed to flies.”
The room falls silent as McKay reins in his finger. He leans forward, linking his hands and resting his elbows on the table. “You will find in my report a summary of the state of their premises five years ago. Nothing of substance has changed. Unfortunately, Gordon and Sparling are not alone. Too many of the enlightened and independent butchers of Saskatoon have seen fit to pretend to regard our regulations as impossible, oppressive, and in a final absurdity, interfering with their civic rights. I can assure you, gentlemen, that in trying to protect the public from the sale of diseased, decomposing, or infected meat, your officials have had to put up with much impudence, insult, and abuse from the members of this trade.”
McKay shrugs. “It is perhaps expecting too much in asking this generation of butchers to come up to any reasonable standard of sanitation. Life is too short to hope to teach men so little ashamed of their unsavoury surroundings.”
As a medical health officer in the early years of the twentieth century, McKay was prepared to use education, persuasion, threats, or unleashed sarcasm to get people to obey health regulations.
Since the middle of the nineteenth century, in the overcrowded cities of Europe and North America, public health had shifted from isolating sick individuals to halt the spread of disease to recognizing the importance of sanitation in reducing diseases and their transmission.
Health became a social, not just an individual, responsibility, and public boards and agencies were established as a result. However, though Louis Pasteur had confirmed the link between germs and disease in the late nineteenth century, many people remained unconvinced.
In Saskatoon, dealing with the underside of the biggest population boom in the history of western Canada, McKay faced a double challenge: enforcing public health standards and convincing people of their necessity. Laws alone, he knew, were no guarantee for progress.
In 1905 the provinces of Alberta and Saskatchewan were carved from the North-West Territories. Five years later, the prairie economy was riding the crest of a worldwide economic wave. Farmers rolled newly mechanized equipment across the plains, anxious to break the soil and begin planting the grains they would export to the world.
Urban emigrants joined them, spilling off the trains to try to make their fortune in the handful of cities and numerous smaller communities sprouting up along the tracks between the Ontario border and the foothills of the Rockies.
Only a relative few realized their dreams of wealth. Although houses and businesses sprang up as quickly as the lumber arrived for their construction and solid four-storey brick office buildings were completed in months, the supply of materials and workers couldn’t keep up with the demand.
Rampant speculation drove up the price of land and made lots inaccessible for many. Rooming houses crammed in dozens of single men, often those from eastern Europe who arrived without competence in the English language and found themselves in the lowestpaid labouring positions.
Others, including white-collar workers and families with children, lived for months in tents.
Municipal politicians poured everything they could muster into the modern conveniences expected in an early twentieth-century city: paved streets and concrete sidewalks, electrical lines and transit tracks, and miles and miles of water and sewer mains.
To manage these services they hired administrators and engineers and, to meet the requirements of the provincial Public Health Act, a medical health officer.
Public health legislation predated Saskatchewan’s incorporation. In 1871, under the North-West Territorial Council, boards of health were established to try to reduce the death toll from the frequent epidemics of smallpox, typhoid fever, tuberculosis, diphtheria, and other diseases that erupted across the plains. In the absence of medical services, the work of isolation and control fell largely on clergy and officers of the North-West Mounted Police.
In 1905, through its Department of Agriculture, the new province established a laboratory partly devoted to disease control: it could analyze diphtheria cultures as well as run tests for seed germination and swamp fever in horses. A provincial MHO was responsible for generating public support for improvements in water and sewage facilities, isolation wards in hospitals, and the collection of data on vital statistics.

The provinces of eastern Canada had more experience dealing with epidemics. Since the mid-1700s occasional legislation had been passed to deal with the temporary ravages of communicable diseases when, for instance, infected persons disembarked ships.
Ontario had its first public health act in 1849 and its first permanent provincial board of health in 1882. A year later, a medical health officer was appointed in Toronto. Other cities followed.
Sanitation issues were often the most immediate concerns of early MHOs. They pressed for a clean water supply and safe, sanitary waste disposal. They wanted lanes and alleys kept clear of manure and discarded materials that might harbour vermin. They requested systematic sanitation and health legislation.
For guidance they looked to Great Britain or the United States where the American Public Health Association had been formed in 1872.
While provincial or municipal laws gave them some powers of enforcement, early MHOs generally relied on education and persuasion to change people’s attitudes and practices. Municipal politicians unwilling to offend their electorates preferred these methods as well.
When trying to prevent infectious diseases, however, a patient approach can have tragic consequences. Long before the second decade of the twentieth century, for instance, clean water and sanitary waste disposal had been identified as the essential elements in halting the spread of typhoid fever.
Still, some families and municipalities continued dangerous practices. In 1911, typhoid fever swept through Ottawa, killing 52 people and infecting 901 in the first three months of the epidemic. Perhaps because it was Ottawa, an inquiry was established to investigate the outbreak.
The cause? Backyard privies in some neighbourhoods were shared by a number of families, and the structures were incapable of handling the resulting quantities of human waste. The overflowing privies polluted a water table and a stream that flowed into the Rideau River above the water intake.
Out in Saskatoon, Dr. McKay considered the Ottawa epidemic inexcusable. He was asked if it could be repeated in his jurisdiction.
Absolutely not, he replied. Saskatoon now had an effective disinfecting and filtration system and a proper water intake. That the western city invested in such a plant could be attributed to McKay’s determination and unflagging persistence.

Born in Huntingdon, Quebec, in 1874, a young William John McKay moved to Morden, Manitoba, with his parents. He graduated from the Manitoba Medical College in 1899. His first practice, which included some work in rural public health, was in Winkler, Manitoba. Four years later he married Susanna Peters and the couple moved to Saskatoon, then a small town of a few hundred people.
The city records are unclear on the date of his first appointment, but within a couple of years of his arrival he took over the part-time position of medical health officer from another physician while continuing to maintain a private practice.
In 1906, Saskatoon, with a population of three thousand, incorporated as a city. It passed a public health bylaw that dealt with wells, water, sewer connections, and the control of communicable diseases, and included provisions to enforce compliance.
Three years later, Saskatchewan passed its first public health act. McKay was asked to sit on the newly formed Council for Public Health, which gave guidance to the provincial health commissioner.
In 1910 when the boom erupted, Saskatoon grew to 12,000 people. Health and Sanitation Department matters consumed more and more of McKay’s time.
His staff now tested the products of all milk vendors in the city and published a scorecard in the local newspapers. Not all of the vendors passed, and McKay encouraged housewives to themselves pasteurize any milk consumed by their families.
The department employed a sizable maintenance staff. Teams of horses and wagons were used to collect garbage and night soil stored in the box closets (privies) used by households without indoor plumbing. More teams routinely cleaned the newly paved streets and tried to keep up with the refuse — waste paper, broken boxes, and dodgers (what we now call fliers) — that littered streets and back lanes.
In January 1911, McKay became a full-time MHO. Meanwhile, the population boom continued. By late 1912 Saskatoon was home to 27,000 people.
Under McKay’s supervision, public health inspectors made frequent visits to food wholesalers and retailers. Their actions often made newspaper headlines.
In June 1912, seven tons of strawberries shipped to the city in a railway car with inadequate ice were found unfit for human consumption and destroyed. The next month fourteen tons of watermelons ended up at the nuisance grounds. In October a similar fate befell twelve tons of B.C. plums.
The annual inspection of the Gordon and Sparling slaughterhouse found the same outrageous conditions of a year earlier. Meanwhile, McKay caught wind of a petition organized by some restaurant owners to have abolished the section of the health bylaw that prohibited restaurants from using basement rooms to store or prepare food.
He told reporters he had never seen a basement in any restaurant or hotel in the city that was fit for these activities.
“The man on the street ... does not want his milk or his meat kept in a damp, mildewed, often flooded cellar,” he said, adding that it was a small group of men trying to bulldoze the petition through council. He was prepared to name names. Not that the city fathers were exempt from his criticism.
The unsanitary state of their nuisance grounds, jail, and, especially, horse stables showed, he said, near “criminal carelessness.”
In August 1912, public health officers discovered a young boy suffering from scarlet fever in a small, unsanitary lean-to at the back of a clothing store. McKay took the opportunity to point out the city’s failure to establish a proper infectious-disease hospital.
Something, he said, will have to be done for those suffering, especially in shacks or boarding houses, “and I don’t see that the city is doing very much to help them.”
That same month, McKay reported that in the previous three weeks ten babies had died of cholera infantum (summer complaint) or similar diseases.
“These babies have died as a direct result of bad food,” McKay said, “particularly bad milk,” which had become dirty by carelessness in production, delivery, or home storage. By early fall, McKay had hired a bacteriologist to analyze samples of water, milk, and other foods.
A local newspaper delighted in its description of the scientist’s ability to count and identify millions of bacteria in a milk sample. His work, it was reported, led to the quick identification of the particular equipment in a dairy that required better sterilization.

McKay brought a public health nurse on staff as well. Her responsibility lay in ensuring adequate medical care for children and mothers, and “relief” for families without an employed father.
On another front, McKay advocated what we now call healthy lifestyles. He encouraged children and adults to be active in sports, including his favourite, golf. He and the city engineer designated a river location for summertime swimming and a riverbank hill for winter sliding.
He suggested that the steam used in the generation of electricity at the city-owned powerhouse be diverted into a public steam bath.
McKay’s tenure was brief. In the fall of 1912 the Daily Star reported that he had ambitions to become a health commissioner in charge of a larger jurisdiction.
At the same time, he decided to travel to England and Europe to pursue postgraduate work in public health. He submitted his resignation and offered to return in one year.
Not surprisingly, some councillors were pleased to accept his resignation. In the end, council granted him a leave. Reviewing his successes on the eve of his departure, the Daily Star wrote: “A man less vigorous and persistent in method and less consistent at heart could not have made such headway.”
While he kept in contact with some of his fellow physicians, little was heard of McKay for the first months he was away. Then, on August 6, 1913, the local press stunned Saskatoon with the news that the doctor had taken ill on a holiday trip to Ireland. He had hurriedly been transported to London for treatment but died within days of what was referred to at the time as pleurisy. He was thirty-nine years old.
The wells question
An ongoing dispute over water and sewer connections that pitted Dr. McKay against city council and some businessmen and homeowners was well documented on the pages of Saskatoon’s two daily newspapers as the “wells question.”
In the early years of the settlement, families and businesses had wells on their properties to provide water for themselves and, often, for their animals. These wells were sometimes sheltered in basements, where the water was pumped manually or raised by rope in buckets. These shallow wells were susceptible to contamination, largely from surface runoff or subsurface water polluted by pit privies or livestock.
As the village turned into a town then quickly burst into a booming city, water and sewer mains were laid under the streets. Bylaws stipulated that a new building constructed where lines already were present had to be hooked up to the mains. Once the pipes had been laid, connections were to be made to all the buildings.
The majority of property owners were happy to oblige. But some resisted. They found the cost too great a hardship. They did not see the need to change from their traditional means of supply. Or they simply didn’t like being told what to do.
In the summer and early fall of 1912, the situation grew tumultuous. Dr. McKay went on the offensive, firing off a torrent of notices to well owners giving them three days to change their water supply.
Accompanied by a gang of men and teams of horses hauling wagons filled with dirt, health inspectors set out at 5:30 in the morning. The newspapers reported what they found: “surface wells of the worst possible type … In nearly all the cases the wooden crib was rotten or mouldy ... in most instances the ordinary bucket was in operation.”
The crews threw disinfectant into the well water and filled in the hole.
Some citizens circulated a petition demanding the health department stop. The raids continued, the inspectors resorting even to subterfuge to root out every well.
On one occasion a Mr. Thomas Ellis complained to city council that a man had come to his house and asked him for a drink. It happened that Mr. Ellis had a well concealed in his basement and no sooner had he given the man the drink than the fellow identified himself as a health inspector and immediately proceeded to fill the well.
It had been, Mr. Ellis said, “the best in the city and as fine as anyone would want to drink out of.” McKay retorted that he knew of a boy who had drunk water out of the well and been taken to the hospital with typhoid fever within a few days.
Still there were those who did not submit. In October, a Mr. John Wilkie was alleged to have assaulted health inspector Fred Dudley as the latter attempted to close Mr. Wilkie’s well.
“The officer,” reported the Daily Star, “is slightly nursing a stiff neck as the result of being grabbed by the coat collar and shaken like a cyclone whirls its human prey. Witnesses of the exciting episode state that the officer was threatened with an axe.” Mr. Wilkie was later convicted of illegally reopening his well instead of having his premises connected to the mains.
While numerous wells were filled in during this campaign, it was years before the last one, like the last outdoor privy, was abandoned.
Themes associated with this article
Advertisement
You might also like...
Canada’s History Archive, featuring The Beaver, is now available for your browsing and searching pleasure!










